Current issue
- Page Path
- HOME > Browse Articles > Current issue
Editorial
- Editorial for Urogenital Tract Infection 2025 Vol. 20 No. 3 - Highlights of This Issue’s Papers and the Urogenital Tract Infection Editors’ Pick
- Jae Min Chung, Koo Han Yoo
- Urogenit Tract Infect 2025;20(3):121-122. Published online December 31, 2025
- DOI: https://doi.org/10.14777/uti.2025edi03
- 604 View
- 7 Download

Review Articles
- Adult Syphilis: A Narrative Review of Clinical Insights and Public Health Implications in Urology
- Seung-Ju Lee, Jin Bong Choi
- Urogenit Tract Infect 2025;20(3):123-131. Published online December 31, 2025
- DOI: https://doi.org/10.14777/uti.2550039017
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
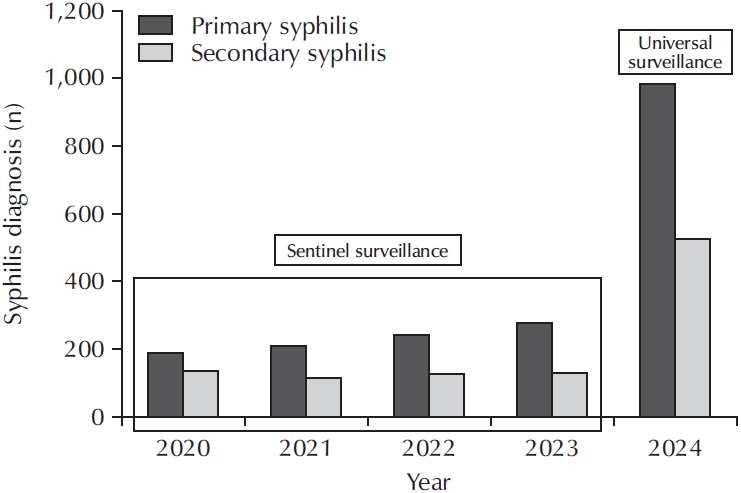
ePub - Syphilis continues to pose a major global public health concern, with more than 7 million cases reported worldwide in 2022, and its incidence continues to rise in numerous regions. In Korea, the shift from sentinel to universal notification in 2024 has revealed a markedly greater disease burden, particularly among men who have sex with men and among younger adults, underscoring changing epidemiological patterns and the urgent need for revised control strategies. In urological practice, syphilis presents with a wide range of often misleading symptoms, including painless genital ulcers, urethritis, and sexual dysfunction, that frequently resemble other genitourinary disorders and complicate diagnostic evaluation. Accurate identification relies on integrating a thorough clinical assessment with serologic testing while remaining alert to diagnostic challenges such as early latent infection, serofast states, and human immunodeficiency virus coinfection. Penicillin G remains the mainstay of therapy, with treatment regimens tailored to the stage of disease and to the presence or absence of central nervous system involvement. Effective partner notification, targeted screening, and consistent follow-up are essential to prevent reinfection and limit further transmission. At a public health level, a multifaceted strategy—strengthened surveillance systems, focused testing in high-risk populations, and embedding syphilis screening within broader sexually transmitted infection care frameworks—is critical to curbing its resurgence. In summary, prompt recognition, adherence to evidence-based management, and coordinated public health measures, together with ongoing advances in diagnostics and prevention, remain fundamental to reducing the continued spread of syphilis and mitigating its impact on both individual and population health.
- 321 View
- 6 Download

- Beyond the Number: Interpreting Prostate-Specific Antigen Elevation in the Context of Prostate Inflammation
- Byoungkyu Han, Ki-Hyuck Moon
- Urogenit Tract Infect 2025;20(3):132-143. Published online December 31, 2025
- DOI: https://doi.org/10.14777/uti.2550032016
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Prostate-specific antigen (PSA) is indispensable but not cancer specific; inflammation, benign prostatic hyperplasia, urinary retention, ejaculation, and instrumentation can all elevate PSA and complicate cancer risk assessment. This review synthesizes current evidence and guidelines to support clinicians in interpreting PSA elevations when inflammation is present or suspected. Acute febrile urinary tract infection and acute bacterial prostatitis may produce very high PSA values, sometimes exceeding 100 ng/mL, and normalization can be slow; therefore, PSA testing during active infection is discouraged. When PSA is only mildly to moderately elevated, standardized repeat testing is essential because a meaningful proportion of results normalize on retesting. A magnetic resonance imaging (MRI)-first pathway improves detection of clinically significant prostate cancer while reducing overdiagnosis and enables biopsy deferral after a negative MRI under structured monitoring. PSA density (PSAD) further refines triage alongside MRI, with practical working thresholds of roughly 0.10–0.20 ng/mL/cm3 calibrated to MRI quality and pretest risk. However, asymptomatic histologic prostatitis (National Institutes of Health category IV) is common and may raise PSA without reliably altering PSAD, which means that PSAD alone cannot confirm that an elevation is attributable solely to inflammation. Validated secondary biomarkers (e.g., Prostate Health Index, 4Kscore, IsoPSA [isoform PSA], Stockholm3, Proclarix, PCA3 [prostate cancer gene 3], SelectMDx [select molecular diagnostics], ExoDx [exosome diagnostics], MPS/MPS2 [MyProstateScore/MyProstateScore 2.0]) are best used selectively when MRI is negative or equivocal and clinical risk remains uncertain. A pragmatic sequence—confirm, image, and refine—helps minimize missed clinically significant cancer while reducing unnecessary antibiotics and biopsies when inflammation is the predominant driver of PSA elevation.
- 386 View
- 13 Download

- Regenerative Medicine for the Kidney
- Vladimir Mashanov, Ji Hyun Kim
- Urogenit Tract Infect 2025;20(3):144-158. Published online December 31, 2025
- DOI: https://doi.org/10.14777/uti.2550028014
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
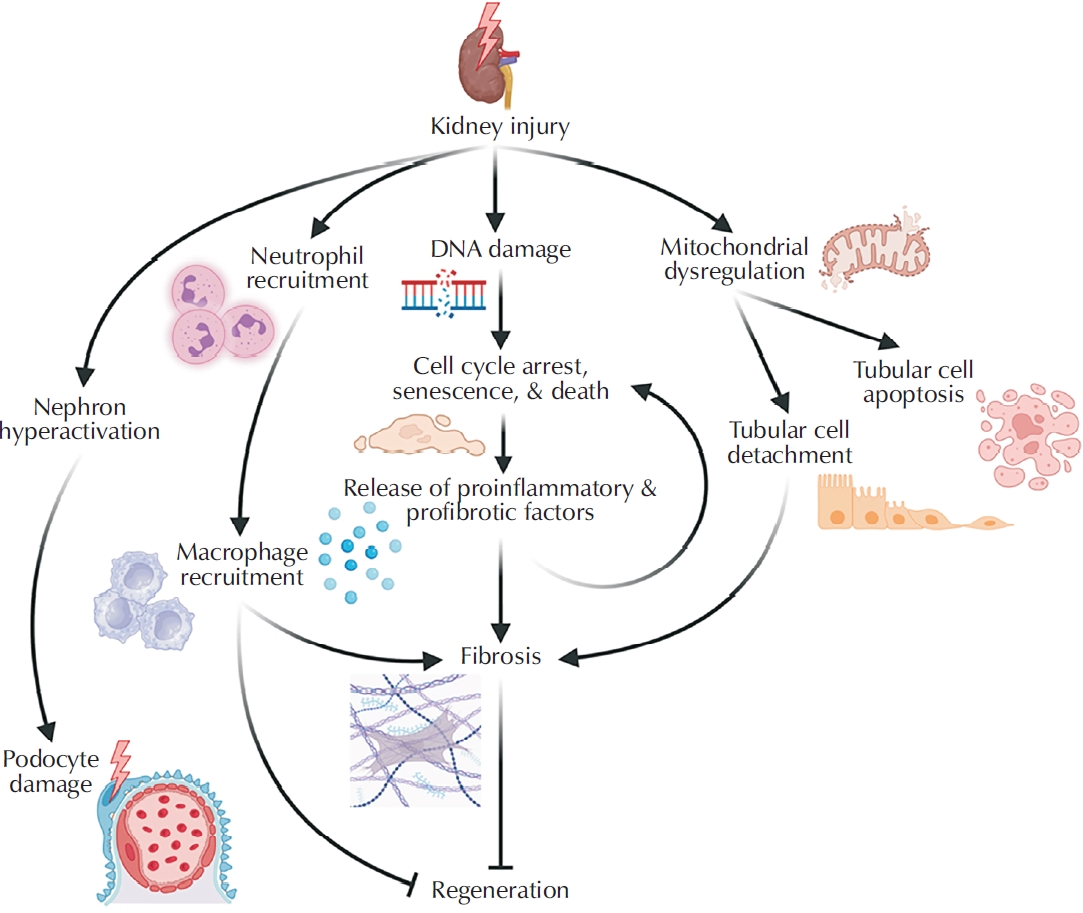
ePub - Kidney disease poses a major and growing global health challenge, with both prevalence and mortality continuing to rise. Current standard-of-care treatments, including dialysis and kidney transplantation, have significant limitations and do not adequately meet clinical needs. This unmet need has driven the development of next-generation regenerative medicine strategies, which can be broadly categorized into 3 areas: (1) approaches that enhance the kidney’s limited intrinsic regenerative capacity; (2) stem cell-based therapies; and (3) implantable bioengineered kidney constructs. This review summarizes recent advances in each of these domains and discusses the major biological, technical, and regulatory challenges that must be addressed to enable successful clinical translation.
- 330 View
- 7 Download

Original Article
- Clinical Characteristics and Risk Factors of Fournier Gangrene: A 15-Years Multicenter Retrospective Study in Korea
- Seung-Kwon Choi, Sin Woo Lee, Hyung-Lae Lee, Jeong Woo Lee, Jung Sik Huh, Yeonjoo Kim, Sangrak Bae, Tae-Hyoung Kim
- Urogenit Tract Infect 2025;20(3):159-166. Published online December 31, 2025
- DOI: https://doi.org/10.14777/uti.2550036018
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader ePub
ePub - Purpose
Fournier gangrene (FG) is a rare but life-threatening necrotizing infection requiring prompt recognition and intervention. This multicenter study aimed to investigate the clinical characteristics, treatment outcomes including mortality, and risk factors associated with death among patients with FG over the past 15 years in Korea. Materials and Methods: We retrospectively reviewed 84 patients diagnosed with FG between 2008 and 2022 across 7 hospitals. Demographics, comorbidities, laboratory findings, and clinical outcomes were analyzed. Mortality-related risk factors were assessed using univariate and multivariate logistic regression analysis.
Results
The mean age was 58.1±15.9 years, and 95.2% of patients were male. Diabetes mellitus (42.9%) and hypertension (36.9%) were the most prevalent comorbidities. Sepsis developed in 38.1% of patients, and the overall mortality rate was 14.3%. In univariate analysis, age ≥70 years, low body mass index, diabetes mellitus, low hemoglobin, low hematocrit, high respiratory rate, and Fournier gangrene severity index (FGSI) ≥9 were significantly associated with mortality. After data correction and multivariate adjustment, diabetes mellitus (odds ratio [OR], 39.61; 95% confidence interval [CI], 2.39–656.32; p=0.010) and respiratory rate (OR, 1.44; 95% CI, 1.09–1.91; p=0.011) were identified as independent predictors of mortality. FGSI≥9 demonstrated borderline association with mortality (p=0.08), indicating its potential clinical relevance.
Conclusions
In this multicenter Korean cohort, the mortality rate of FG remained substantial at 14.3%. Diabetes mellitus and elevated respiratory rate were independent predictors of mortality, while FGSI≥9 demonstrated a borderline yet clinically meaningful association, suggesting its role as a useful severity indicator in early risk stratification.
- 247 View
- 9 Download

Case Report
- Primary Bladder and Ureteral Amyloidosis Initially Diagnosed as Chronic Cystitis: A Case Report
- Seungsoo Lee, Dan Bee Lee, Hyun Jung Lee, Won Hoon Song, Sung-Woo Park, Jong Kil Nam
- Urogenit Tract Infect 2025;20(3):167-172. Published online December 31, 2025
- DOI: https://doi.org/10.14777/uti.2550038019

-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
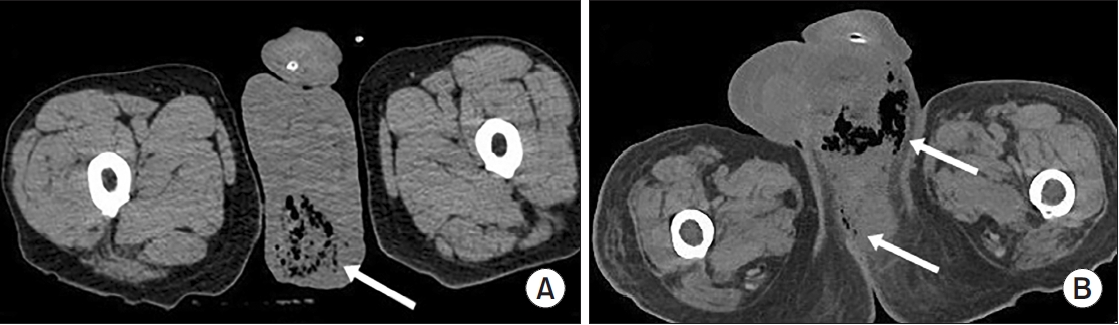
ePub - Primary localized amyloidosis confined to the urinary tract is uncommon and frequently misinterpreted due to clinical and radiologic overlap with more prevalent conditions. We describe a 69-year-old woman who experienced recurrent gross hematuria over 2 years and underwent initial transurethral resection based on a presumptive diagnosis of chronic cystitis. Subsequent evaluation revealed a left ureteral mass with hydronephrosis, raising concern for malignancy. Histopathologic examination of both bladder and ureteral specimens demonstrated amorphous eosinophilic deposits that stained positive with Congo red and showed apple-green birefringence under polarized microscopy. Immunofluorescence confirmed λ-light-chain predominance, establishing AL (amyloid light chain)-type amyloidosis without systemic involvement. The patient underwent complete endoscopic resection and remains asymptomatic during ongoing surveillance. This case highlights the diagnostic challenges posed by localized urinary amyloidosis and underscores the importance of histologic confirmation in atypical inflammatory lesions.
- 315 View
- 4 Download

Letter to the Editor
- A Commentary on “Diagnostic Utility of the Sysmex UF-5000 Flow Cytometer in Acute Bacterial Prostatitis: A Retrospective Pilot Study”
- Dong-Hoon Lim
- Urogenit Tract Infect 2025;20(3):173-174. Published online December 31, 2025
- DOI: https://doi.org/10.14777/uti.2550044022
- 164 View
- 7 Download


 KAUTII
KAUTII


 First
First Prev
Prev


