Funded Articles
- Page Path
- HOME > Browse Articles > Funded Articles
Review Articles
- Beta-Lactamase-Mediated Antibiotic Resistance in Urinary Tract Infections: Mechanisms and Therapeutic Strategies
- Fanglin Shao, Dengxiong Li, Jie Wang, Zhouting Tuo, Zhipeng Wang, Wuran Wei, Ruicheng Wu, Dechao Feng
- Urogenit Tract Infect 2025;20(2):67-81. Published online August 31, 2025
- DOI: https://doi.org/10.14777/uti.2550012006
-
 Abstract
Abstract
 PDF
PDF PubReader
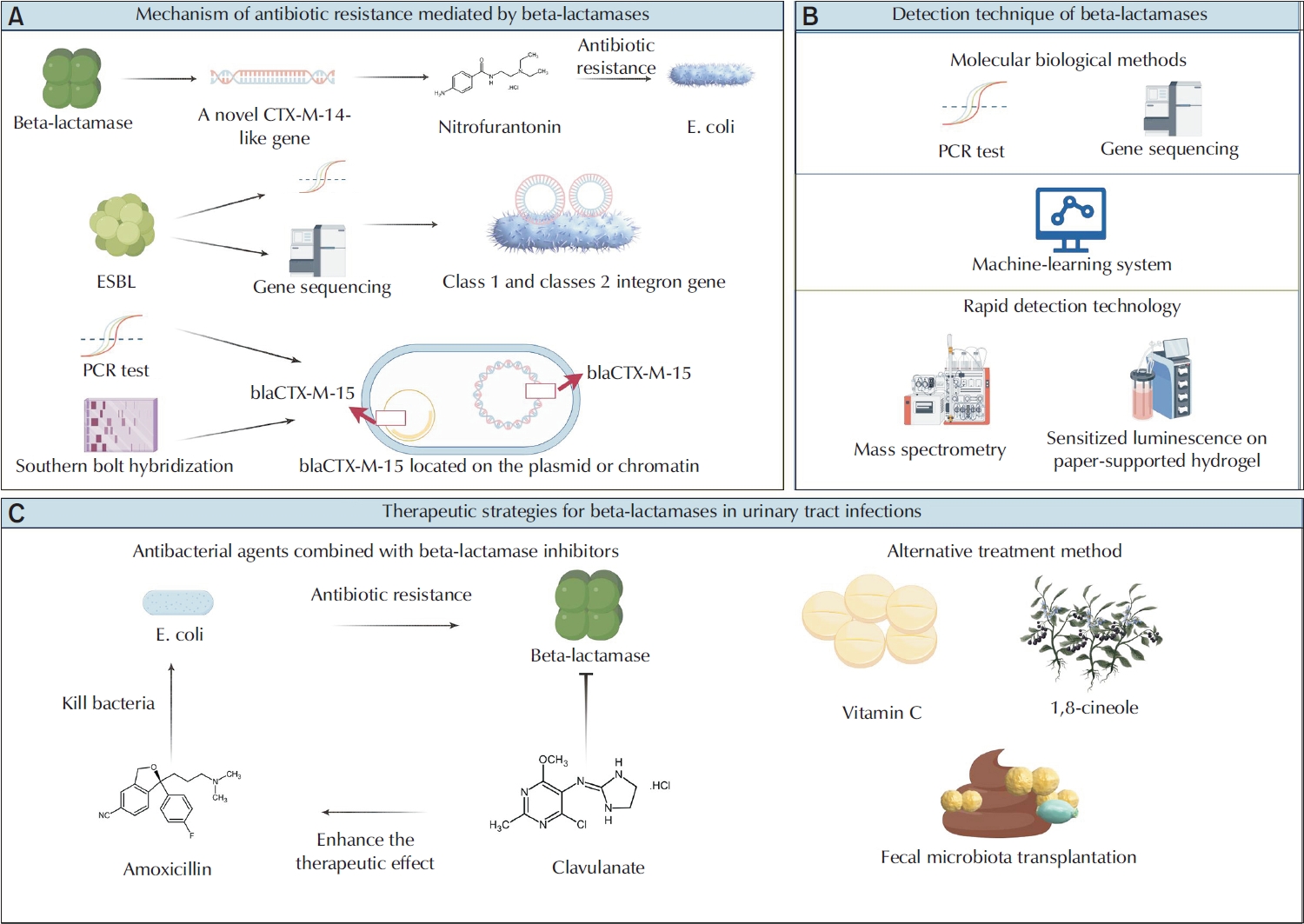
PubReader - Urinary tract infections (UTIs) are among the most prevalent bacterial infections globally, and are primarily caused by Escherichia and Klebsiella. The overprescription and inappropriate use of antibiotics have accelerated the emergence of multidrug-resistant bacteria. Beta-lactamases play a critical role in mediating antibiotic resistance in UTIs. These enzymes promote bacterial resistance through multiple mechanisms, including gene mutation, plasmid-mediated horizontal gene transfer, and the involvement of integrons. Comprehensive knowledge of the ways in which beta-lactamases contribute to resistance in UTIs is essential for improving treatment strategies. Advances in detection technologies, such as gene sequencing and mass spectrometry, have greatly enhanced the ability to monitor and predict bacterial resistance. Current therapeutic strategies include the application of beta-lactamase inhibitors, the development of novel antibiotics, and alternative treatments that have shown efficacy against beta-lactamase-mediated antibiotic resistance. This paper reviews the mechanisms of beta-lactamase-mediated resistance in UTIs and provides an in-depth overview of several detection methods and therapeutic approaches.
-
Citations
Citations to this article as recorded by- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(2): 55. CrossRef
- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 6,577 View
- 74 Download
- 1 Crossref

- Molecular Mechanisms of Antibiotic Resistance in Uropathogenic Escherichia coli: A Narrative Review
- Nakjun Choi, Dong Uk Kim, Eun-Jin Lee
- Urogenit Tract Infect 2025;20(2):96-106. Published online August 31, 2025
- DOI: https://doi.org/10.14777/uti.2550018009
-
 Abstract
Abstract
 PDF
PDF PubReader
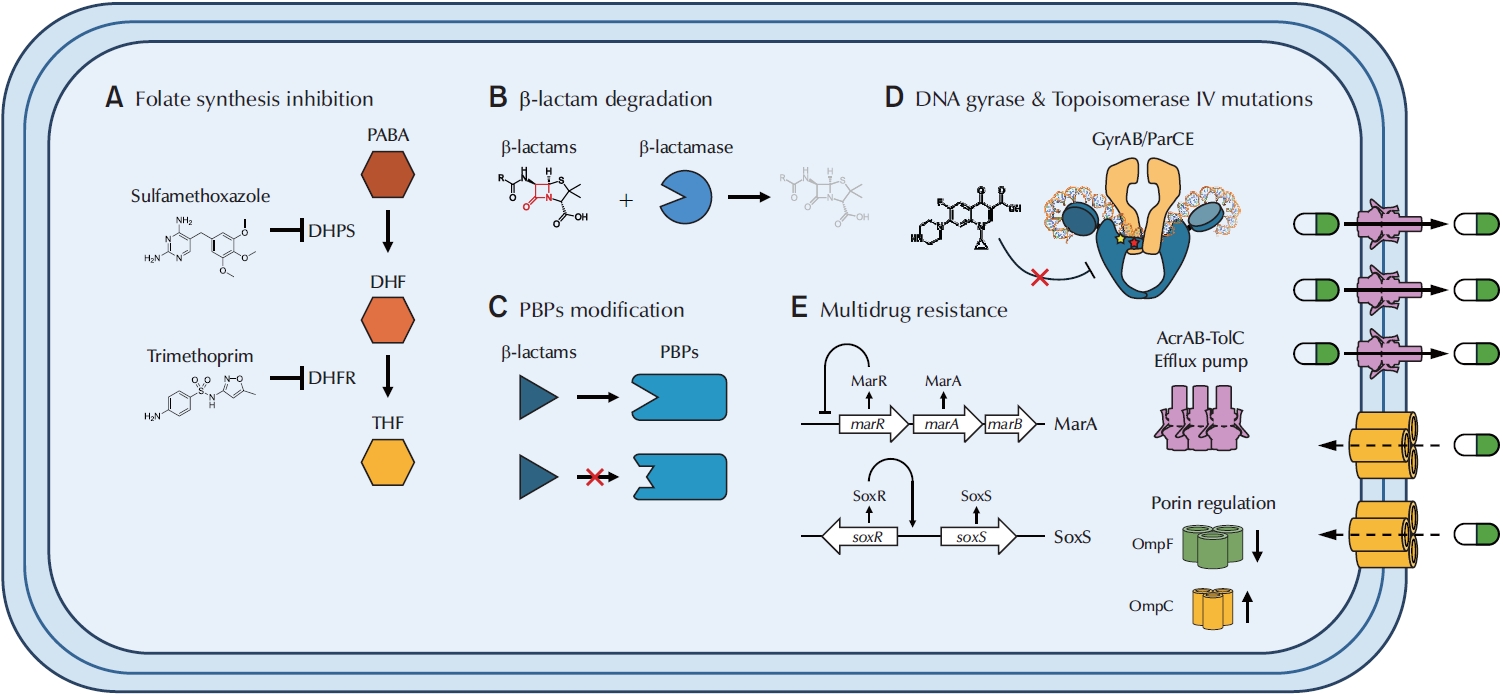
PubReader - Urinary tract infections (UTIs) are among the most prevalent bacterial infections worldwide, with uropathogenic Escherichia coli (UPEC) serving as the primary causative agent. Although antibiotic therapy remains the standard of care for UTI treatment, the increasing prevalence of antimicrobial resistance has substantially reduced the effectiveness of commonly prescribed antibiotics. Resistance to trimethoprim-sulfamethoxazole (TMP-SMX), β-lactams, and fluoroquinolones is particularly concerning, as these agents constitute the principal therapeutic options for UTIs. This review examines the molecular mechanisms underlying UPEC resistance to these three classes of antibiotics, including target site modifications, efflux pump overexpression, porin regulation, and enzymatic degradation. Furthermore, it explores how these resistance determinants contribute to the development of multidrug-resistant (MDR) UPEC strains, which demonstrate cross-resistance to multiple antibiotics and present significant challenges for clinical management. Novel therapeutic strategies, such as efflux pump inhibitors, bacteriophage therapy, and genomic-guided precision medicine, are under investigation as potential solutions to address the growing global burden of MDR UPEC, alongside alternative non-antibiotic treatments. This review aims to provide a comprehensive overview of the genetic and regulatory pathways driving antibiotic resistance in UPEC, offering insights that may guide the development of effective treatment strategies and help mitigate the ongoing spread of antimicrobial resistance.
-
Citations
Citations to this article as recorded by- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(2): 55. CrossRef
- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 6,014 View
- 113 Download
- 1 Crossref

Original Article
- Diagnostic Utility of the Sysmex UF-5000 Flow Cytometer in Acute Bacterial Prostatitis: A Retrospective Pilot Study
- Young Kyu Han, Jeong Woo Lee, Hae-Il Park, Jin Bong Choi
- Urogenit Tract Infect 2025;20(2):107-113. Published online August 31, 2025
- DOI: https://doi.org/10.14777/uti.2550022011
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader - Purpose
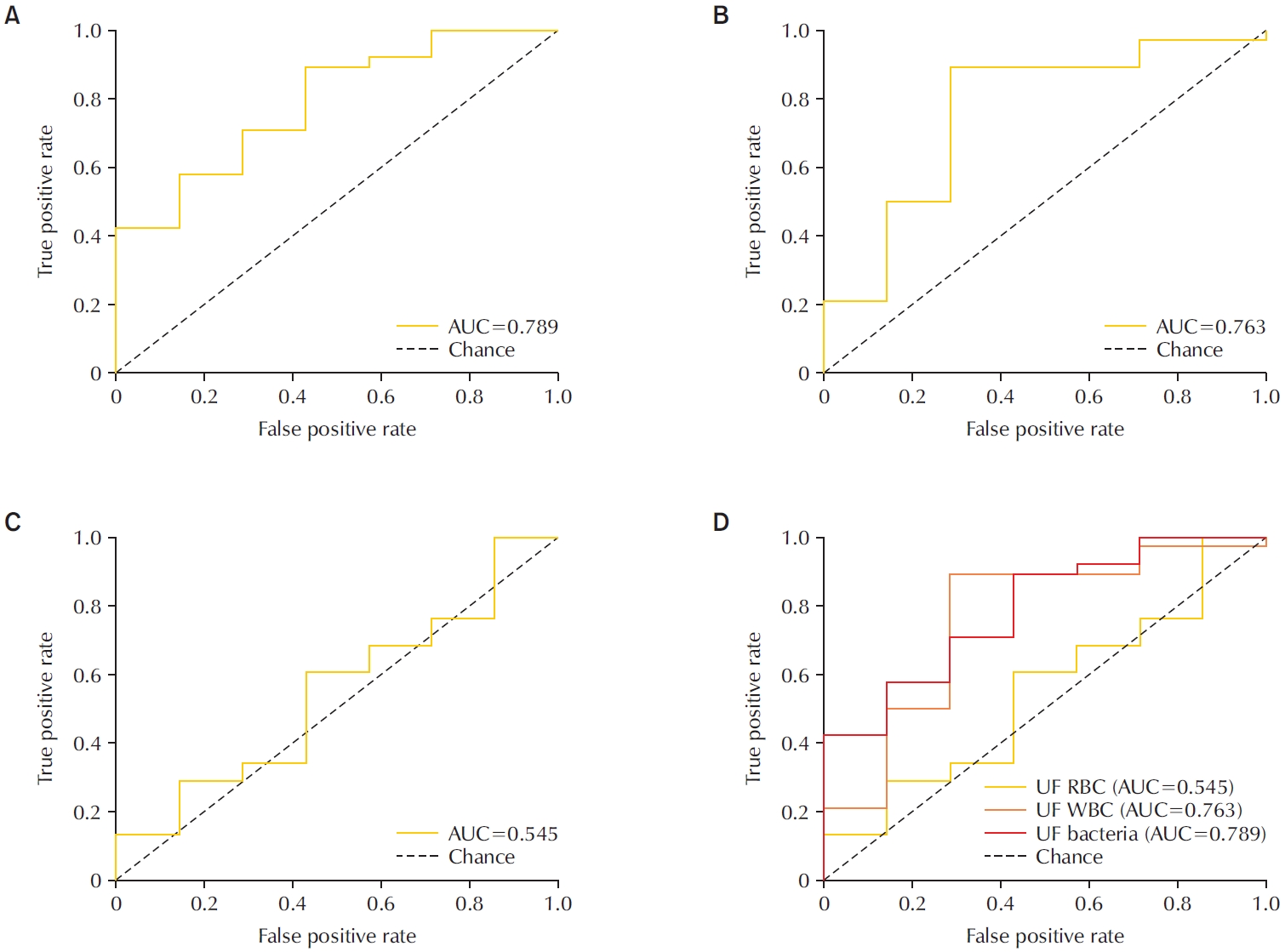
To evaluate the diagnostic performance of the Sysmex UF-5000 flow cytometer in detecting acute bacterial prostatitis (ABP) compared to standard urine culture. Materials and Methods: This retrospective study analyzed 45 urine samples from patients with a clinical diagnosis of ABP. Each sample was evaluated using the UF-5000 to measure red blood cells (RBC), white blood cells (WBC), and bacterial counts, and the results were compared with those from standard urine culture and Gram staining. Receiver operating characteristic curves were generated, and sensitivity, specificity, positive predictive value (PPV), and negative predictive value were determined. Concordance between Gram classification by the UF-5000 and conventional Gram staining was also evaluated.
Results
Of the 45 patients, 84.4% had positive urine cultures. The bacterial count parameter demonstrated the highest diagnostic performance (area under the curve [AUC]=0.79; sensitivity, 89.5%; PPV, 91.9%), outperforming WBC (AUC=0.76) and RBC (AUC=0.55). The Gram classification flag showed an overall concordance of 85.7% with conventional Gram staining, with a concordance rate of 88% for Gram-negative organisms.
Conclusions
The Sysmex UF-5000 exhibited good concordance with urine culture for patients with ABP, particularly through the bacterial count parameter. Although it does not replace culture, the UF-5000 may serve as a rapid adjunctive tool to support early clinical decision-making in suspected ABP cases. -
Citations
Citations to this article as recorded by- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(2): 55. CrossRef - A Commentary on “Diagnostic Utility of the Sysmex UF-5000 Flow Cytometer in Acute Bacterial Prostatitis: A Retrospective Pilot Study”
Dong-Hoon Lim
Urogenital Tract Infection.2025; 20(3): 173. CrossRef
- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 1,501 View
- 31 Download
- 2 Crossref

Case Report
- Cyclic Hematuria Misdiagnosed as Hemorrhagic Cystitis in a Rare Case of Vesicouterine Fistula Post-Cesarean Section: A Case Report of Youssef Syndrome
- Youngjoo Kim
- Urogenit Tract Infect 2025;20(2):114-117. Published online August 31, 2025
- DOI: https://doi.org/10.14777/uti.2550024012
-
 Abstract
Abstract
 PDF
PDF PubReader
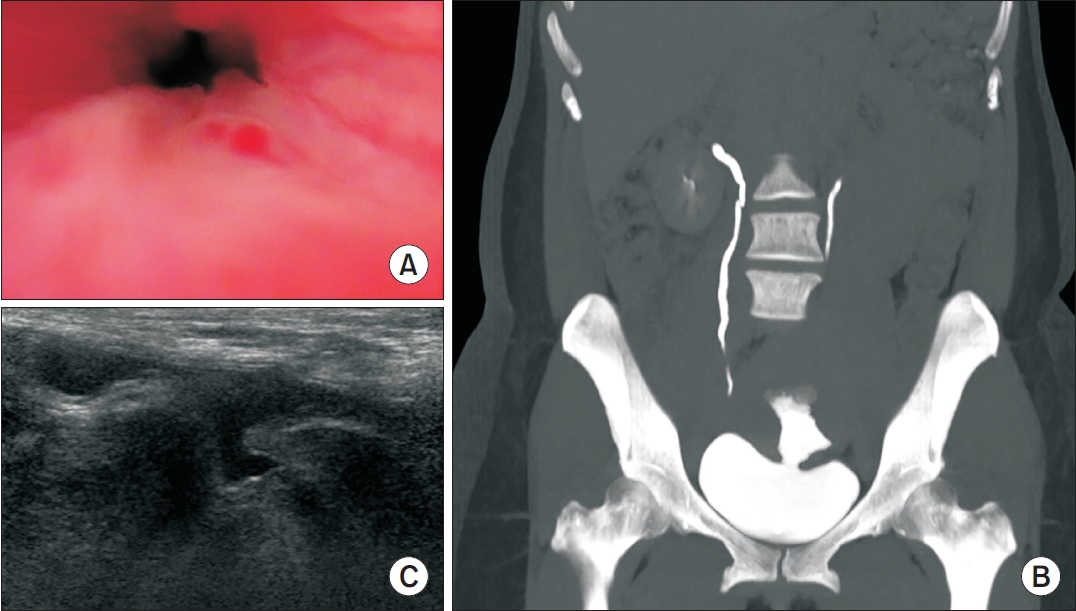
PubReader - Vesicouterine fistulas are rare complications that may occur following cesarean sections and are frequently misdiagnosed due to their diverse clinical presentations. This report presents a case involving a small vesicouterine fistula initially managed conservatively, which later manifested as cyclic hematuria mimicking hemorrhagic cystitis, ultimately leading to a diagnosis of Youssef syndrome. A 45-year-old woman developed persistent vaginal urinary leakage 3 weeks after a cesarean section. Diagnostic evaluation confirmed a small (<1 cm) vesicouterine fistula. Conservative management with Foley catheterization resulted in spontaneous closure. Four months later, the patient experienced cyclic gross hematuria and dysuria without menstruation, and was subsequently diagnosed with Youssef syndrome. Hormonal therapy using continuous oral contraceptives successfully resolved the hematuria, providing a noninvasive therapeutic option. This case highlights the importance of considering Youssef syndrome in patients with cyclic hematuria after cesarean section, in order to distinguish it from hemorrhagic cystitis and ensure timely, appropriate management.
-
Citations
Citations to this article as recorded by- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(2): 55. CrossRef
- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 1,274 View
- 10 Download
- 1 Crossref

Review Article
- Emerging Insights Into Microbiome Therapeutics for Urinary Tract Infections: A Narrative Review
- Hoonhee Seo, Md Abdur Rahim, Indrajeet Barman, Mohammed Solayman Hossain, Hanieh Tajdozian, Fatemeh Ghorbanian, Md Sarower Hossen Shuvo, Jiho Choi, Sukyung Kim, Heejo Yang, Ho-Yeon Song
- Urogenit Tract Infect 2025;20(1):4-16. Published online April 30, 2025
- DOI: https://doi.org/10.14777/uti.2448034017
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Urinary tract infections (UTIs) are among the most common bacterial infections worldwide, affecting millions annually and posing a significant global health concern. Traditional therapies for UTIs are becoming increasingly ineffective due to rising drug resistance and their tendency to disrupt the host's healthy microbiota, leading to further side effects. Consequently, there is an urgent need to develop alternative therapeutic agents that differ from conventional regimens and have fewer or no side effects. In this context, microbiome therapeutics offer a promising solution, given their demonstrated efficacy against various infectious diseases. Advances in scientific technology, particularly next-generation sequencing, have deepened our understanding of urinary microbiome dynamics, revealing a complex interplay within the urobiome that influences the onset and progression of UTIs. Uropathogenic bacteria do not solely cause UTIs; shifts in the composition of the urinary microbiome and interactions within the microbial community, known as host-microbiota interactions, also play a significant role. Although recent studies underscore the potential of targeting the urinary microbiome to manage UTIs and related complications, this field is still emerging and faces numerous regulatory and technical challenges. Further in-depth and comprehensive research is required to advance this pioneering concept into clinical practice.
-
Citations
Citations to this article as recorded by- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(1): 1. CrossRef - Efficacy and safety of N-acetylcysteine vs. probiotics in in-vivo biofilm prevention on ureteral stents: a prospective randomized controlled pilot in vivo study
Iqbal Singh, Himanshu Agrawal, Shailender Maurya, Himanshu Tanwar, Sanjay Gupta, N. P. Singh
International Urology and Nephrology.2025; 58(3): 811. CrossRef
- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 14,233 View
- 169 Download
- 2 Crossref

Original Article
- Efficacy of Urovaxom for Improving Chronic Pelvic Pain Syndrome Symptoms in Prostate Cancer Patients Who Underwent Radical Prostatectomy: A Multicenter, Prospective Cohort Study
- Jun-Koo Kang, Yun-Sok Ha, Sungchan Park, Tae Gyun Kwon, Tae-Hwan Kim
- Urogenit Tract Infect 2025;20(1):42-47. Published online April 30, 2025
- DOI: https://doi.org/10.14777/uti.2550014007
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose
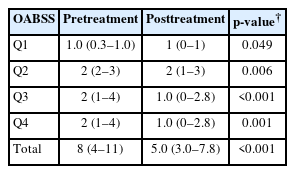
Chronic pelvic pain syndrome (CPPS) is a multifactorial condition that can significantly diminish quality of life. Although some patients have reported persistent pelvic pain after radical prostatectomy (RP), the prevalence and direct causal relationship between CPPS and RP remain unclear. This multicenter prospective study aimed to evaluate the efficacy of Urovaxom for improving CPPS symptoms. Materials and Methods: A total of 52 prostate cancer patients who underwent RP were enrolled and administered Urovaxom (60 mg/day) for 12 weeks. Changes in National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI), overactive bladder symptom score (OABSS), International Prostate Symptom Score (IPSS), and inflammation markers (white blood cell [WBC], C-reactive protein [CRP]) were analyzed using the Wilcoxon signed-rank test.
Results
After 12 weeks of treatment, the NIH-CPSI total score significantly decreased from 19 (interquartile range [IQR], 16–23) to 12.5 (IQR, 8.0–16.8) (p<0.001). The OABSS total score decreased from 8 (IQR, 4–11) to 5 (IQR, 3.0–7.8), and the IPSS total score decreased from 13.5 (IQR, 10.0–22.8) to 10.5 (IQR, 5.0–17.0) (p<0.001). WBC levels showed a slight increase (p=0.028), but the clinical relevance of this change is uncertain and warrants further investigation. CRP changes were not statistically significant (p=0.274).
Conclusions
Urovaxom demonstrated significant efficacy in improving CPPS symptoms, particularly pain and reduced quality of life, in patients following RP. These findings suggest Urovaxom as a potential therapeutic option for CPPS after management using RP. -
Citations
Citations to this article as recorded by- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(1): 1. CrossRef - Addressing an Unmet Need in Postprostatectomy Care: Perspectives on Urovaxom
Byeong Jin Kang
Urogenital Tract Infection.2025; 20(2): 118. CrossRef
- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 5,197 View
- 44 Download
- 2 Crossref

Review Articles
- Mechanistic Insights Into Persistent Bacterial Cystitis as a Basis for Vaccine Development: A Narrative Review
- Karen Serrano-Arevalo, Manisha Naskar, Hae Woong Choi
- Urogenit Tract Infect 2024;19(3):60-72. Published online December 31, 2024
- DOI: https://doi.org/10.14777/uti.2448022011
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
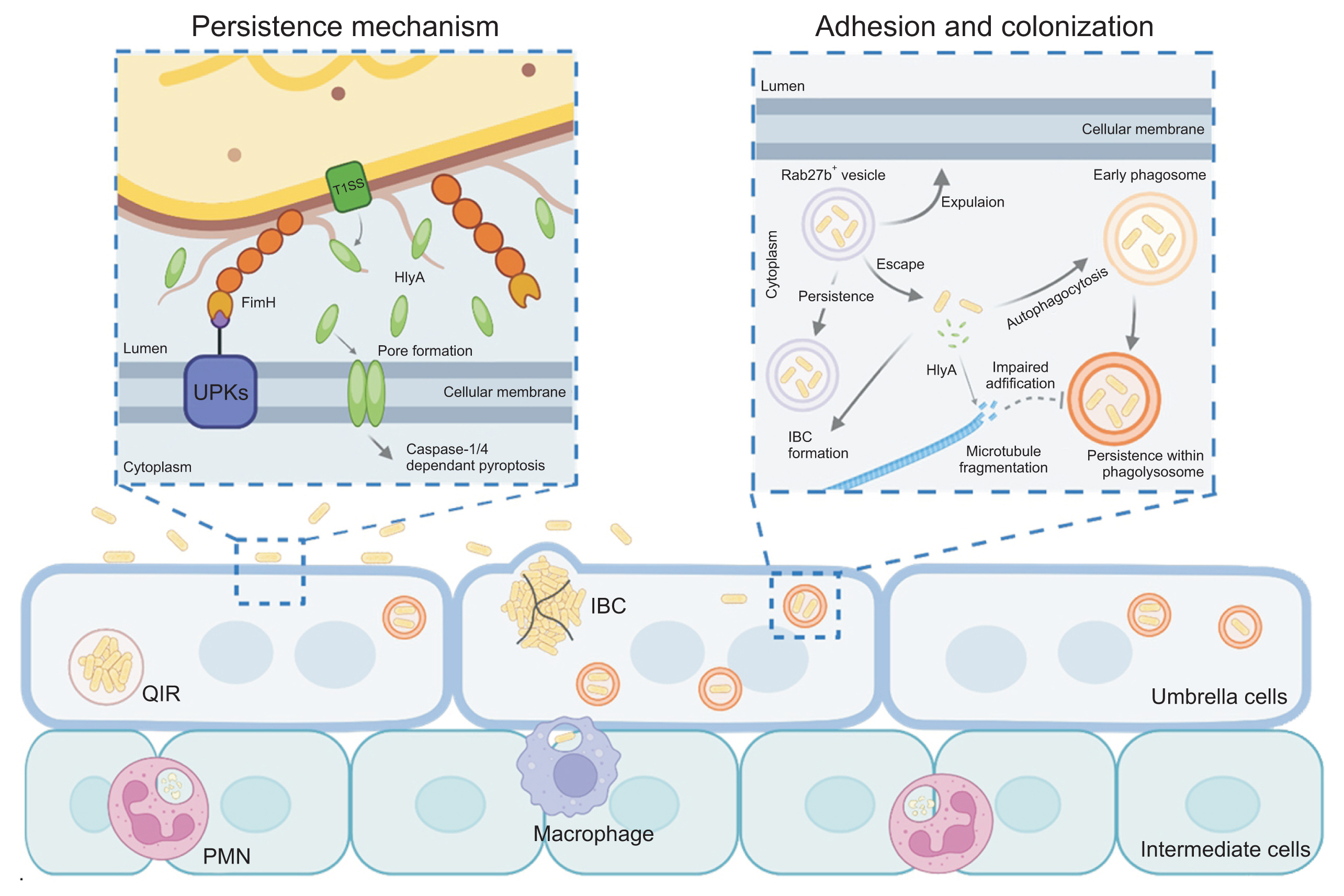
ePub - Urinary tract infections (UTIs) are primarily caused by uropathogenic Escherichia coli (UPEC), which frequently lead to recurrent infections. These bacteria utilize several strategies to establish infection in the host; in particular, virulence factors such as fimbriae and α-hemolysin facilitate persistent infection, evade host immune responses, and minimize antibiotic exposure. To date, antibiotics have been the primary treatment for UTIs. However, an increasing emphasis has been placed on the need for UTI vaccines, with mucosal vaccine products now available in several countries. Additionally, vaccines targeting intracellular UPEC, utilizing adjuvants, are currently under development. Understanding the pathogenic mechanisms of uropathogens has enabled the development of new treatment approaches, paving the way for next-generation preventive and therapeutic methods that could effectively manage recurrent UTIs in the future.
-
Citations
Citations to this article as recorded by- Mechanisms and clinical implications of bacterial persistence in recurrent urinary tract infections
Changil Choi, Dong Soo Kim, Jin Bong Choi, Taesoo Choi, Jeong Woo Lee
Investigative and Clinical Urology.2026; 67(2): 123. CrossRef - Bacterial biofilm – as a contributor to urinary tract infections
Zuzanna Trześniewska-Ofiara, Mariola Mendrycka, Agnieszka Woźniak-Kosek
Biuletyn Głównej Biblioteki Lekarskiej.2025; 58(384): 83. CrossRef
- Mechanisms and clinical implications of bacterial persistence in recurrent urinary tract infections
- 6,800 View
- 58 Download
- 2 Crossref

- Postoperative Microscopic Pyuria and Role of Damage-Associated Molecular Pattern: A Literature Review
- Min-Kyu Kim, Ki Hong Kim
- Urogenit Tract Infect 2024;19(3):73-79. Published online December 31, 2024
- DOI: https://doi.org/10.14777/uti.2448026013
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - All patients who undergo transurethral prostate surgery exhibit pyuria and microscopic hematuria in postoperative urinalysis. Postoperative asymptomatic pyuria is associated with the inflammatory process and surface remodeling of the prostate, rather than infection. Various studies have investigated the incidence, duration, and risk factors for postoperative pyuria, noting that factors like age, surgery time, and prostate size can influence outcomes. Postoperative pyuria reflects tissue recovery and inflammation, and the use of antibiotics in asymptomatic patients may not be appropriate.
- 5,159 View
- 28 Download

Original Article
- Outbreak of Cystoscopy-Related Urinary Tract Infections With Pseudomonas aeruginosa in South Korea, 2022: A Case Series
- Beomsoo Kim, Young-Sin Choi, Jun-Koo Kang, Yun-Sok Ha, Seock Hwan Choi, Bum Soo Kim, Hyun Tae Kim, Eun Sang Yoo, Tae Gyun Kwon, Jae-Wook Chung, Tae-Hwan Kim
- Urogenit Tract Infect 2024;19(3):97-103. Published online December 31, 2024
- DOI: https://doi.org/10.14777/uti.2448028014
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose
This study conducted an epidemiological investigation of Pseudomonas aeruginosa urinary tract infections (UTIs) following cystoscopy at Chilgok Kyungpook National University Hospital. Materials and Methods: From May 16 to July 15, 2022, among 353 patients who underwent cystoscopy, 6 patients reported febrile UTIs following cystoscopy. They were admitted to the urology department of the hospital after visiting the Emergency Department. P. aeruginosa was found in the urine cultures of 4 of the 6 hospitalized patients. During the epidemiological investigation, no changes were observed in factors such as the reprocessing procedures for endoscopic equipment. Therefore, microbiological tests were performed using environmental samples derived from the endoscopic equipment and cleaning process.
Results
P. aeruginosa was identified in a dual-enzymatic detergent (EmPower) used during the endoscope cleaning process. After changing the disinfectant and cleaning process, no further bacterial growth was observed in subsequent microbiological tests.
Conclusions
This study highlights the potential of cystoscopes to serve as reservoirs for bacteria due to inadequate cleaning during the disinfection process. To minimize the risk of infections following cystoscopy, it is important to pay close attention to the reprocessing and cleaning of cystoscopes. -
Citations
Citations to this article as recorded by- A Commentary on “Outbreak of Cystoscopy-Related Urinary Tract Infections With Pseudomonas aeruginosa in South Korea, 2022: A Case Series”
Byoungkyu Han
Urogenital Tract Infection.2025; 20(1): 52. CrossRef
- A Commentary on “Outbreak of Cystoscopy-Related Urinary Tract Infections With Pseudomonas aeruginosa in South Korea, 2022: A Case Series”
- 3,986 View
- 70 Download
- 1 Crossref


 KAUTII
KAUTII

 First
First Prev
Prev


