Abstract
Xanthogranulomatous epididymitis is very rare, and there are few case reports worldwide. Clinically, it is necessary to differentiate between chronic scrotal inflammatory diseases, such as tuberculous epididymitis and testicular tumors. Proteus and Escherichia coli are the pathogens that generally cause xantho-granulomatous pyelonephritis, but the pathogens of xanthogranulomatous epididymitis are unclear. This paper reports a case of a 66-year-old male with epididymitis on scrotal ultrasonography and had Pseudomonas aeruginosa detected in a culture test. An orchiectomy was performed because he did not respond to antibiotic treatment.
-
Keywords: Xanthogranuloma, Epididymitis, Orchiectomy
Xanthogranulomatous inflammation is a rare benign disease resulting in tissue destruction and chronic granulomatous inflammation involving xanthoma cells (lipid-laden macrophage) and plasma cells [
1]. Unlike xanthogranulomatous pyelonephritis, the causative pathogen of xanthogranulomatous epididymitis has not been identified, but a few cases related to
Escherichia coli and
Pseudomonas aeruginosa have been reported [
2,
3]. Accordingly, the authors report a case of xanthogranulomatous epididymitis, which was accompanied by Pseudomonas aeruginosa in urine culture and did not respond to antibiotics, requiring surgical treatment. The possibility of xanthogranulomatous inflammation should be considered for orchitis and epididymitis that do not respond to medical treatment and gradually progresses.
CASE REPORT
A 66-year-old male patient with visual internal urethrotomy (VIU) one month earlier at another hospital visited the authors’ clinic with voiding symptoms after foley removal. A urinary tract infection was found in the urine test. Antibiotics were administered, and culture tests were performed. In addition, cystostomy or foley catheter was recommended, but the patient refused for livelihood reasons. Multi-drug resistant
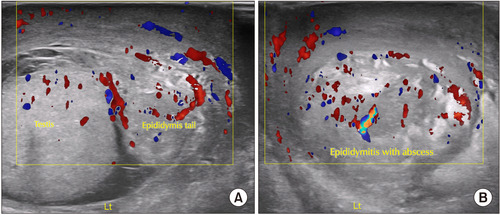
P. aeruginosa was detected in the urine culture and urethral pus culture test. After one week of empirical antibiotic treatment, he complained of severe pain and swelling in the left scrotum, and left epididymo-orchitis with an abscess was suspected on ultrasonography (
Fig. 1A, B).
The patient refused hospitalization and surgical treatment for personal reasons and requested antibiotic treatment. Therefore, an additional three weeks of combined antibiotic treatment (levofloxacin, amikacin, and minocycline) was performed. Despite this, the symptoms worsened, so a scrotal exploration was performed for drainage and partial epididymectomy. Partial necrosis of the testicular surface was observed, and adhesions between the scrotum and epididymal tissue were severe. Simple drainage and accurate excision of the infected tissue were impossible. Therefore, during the operation, there was no choice but to switch to epididymal-orchiectomy.
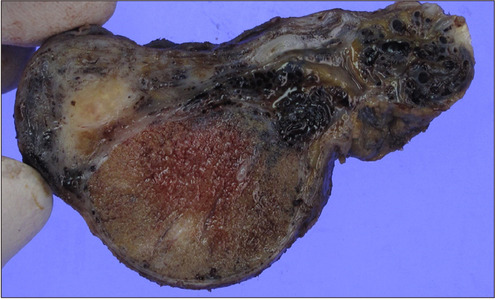
The gross examination showed that the testicle was severely adherent to the surrounding tissue, with partially necrotic tissue observed. The epididymis specimen was severely adherent to adjacent structures and had an enlarged tail portion. The cut surface of the epididymis revealed a yellow nodular lesion measuring up to 1.4 cm in the greatest dimension (
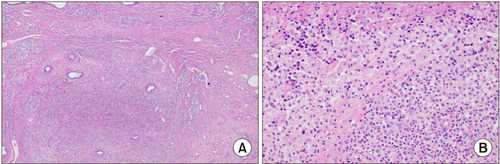
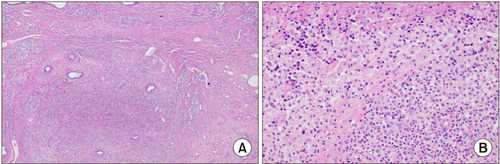
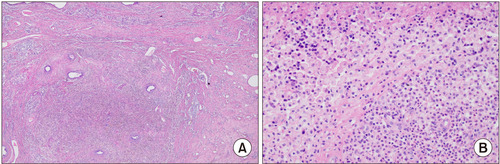
Fig. 2). The histopathology findings showed markedly distorted epididymal tissue replaced with infiltration of inflammatory cells with fibrosis and numerous foamy histiocytes with neutrophils accompanied with necrotic tissue debris (
Fig. 3A, B). Three months after surgery, the patient recovered well, but the urethral stricture recurred, so additional VIU surgery was performed. Authors received informed consent for the use of the patients’ photographs or other information through the publication.
DISCUSSION
Xanthogranulomatous inflammation is a chronic infla-mma-tory disease characterized by severe tissue destruction and replaced with xanthoma cells (lipid-laden macrophages) [
1,
3]. In urology, xanthogranulomatous pyelonephritis is rare but accounts for the majority [
1]. In contrast, xantho-granulomatous inflammation can also occur in the prostate, spermatic cord, testis, and epididymis, but it is extremely rare.
Since Wiener et al. [
4] first reported xanthogranulomatous epididymitis in 1987, 19 and four cases have been reported in the English and Korean literature, respectively [
5-
8]. The risk factors of xanthogranulomatous inflammation are unclear, but chronic inflammation, fat metabolism disorders, congenital malformations, diabetes, and inappropriate use of antibiotics have been associated [
1-
3,
9]. In the case of xanthogranulomatous epididymitis, few cases accompanied by neurogenic bladder have been reported, suggesting that urinary tract infection due to urinary retention is refluxed into the epididymis [
2,
7,
9].
The patient also had a history of an indwelling foley catheter after VIU surgery because of a urethral stricture. Therefore, in this patient's case, a urinary tract infection caused by voiding difficulty plays an important role in the cause of xanthogranulomatous epididymitis. In addition, even after the orchiectomy, urethral stricture continued to recur, and the patient underwent repeated VIU surgery.
The pathogen of xanthogranulomatous pyelonephritis has been reported as
Proteus,
E. coli, and
Aerobacter [
1,
3]. In the case of xanthogranulomatous epididymitis,
E. coli was generally reported, but only one case of
P. aeruginosa has been reported [
2]. The causative organism in the present case was
P. aeruginosa. Nevertheless, the etiology is not limited to infections by specific bacteria, as xanthogra-nulomatous inflammation results from a chronic bacterial infection [
2,
3,
5]. A differential diagnosis of xantho-granu-lomatous epididymitis includes testicular tumors, infectious epididymo-orchitis, malakoplakia, tuberculosis, and idio-pathic xanthoma [
2,
8,
10].
Xanthogranulomatous inflammatory disease can only be confirmed by the histopathology findings. Hence, an aggressive inguinal approach with epididymectomy or radical orchiectomy is the definitive course of treatment in most reported cases [
2,
4-
8]. On the other hand, the current therapeutic approach avoids surgical treatment. In the case of xanthogranulomatous pyelonephritis, there are some reports of successful treatment with antibiotics alone when the lesion is localized [
11]. Nevertheless, a complete surgical resection is the treatment most recommended for xantho-granulomatous epididymitis to differentiate it from testicular neoplasia [
3,
5,
6].
In the present case, after removing the foley catheter indwelled after VIU surgery, the patient visited the authors’ clinic with dysuria and was first diagnosed with a urinary tract infection. Although a P. aeruginosa urinary tract infection cannot be determined definitively as the etiology of xanthogranulomatous epididymitis. The culture test revealed P. aeruginosa as a multidrug-resistant strain that did not respond well to antibiotics. Therefore, the authors are concerned that a more rapid surgical approach should have been taken rather than waiting for a response to antibiotic treatment.
In conclusion, orchitis and epididymitis that do not respond to medical treatment and gradual progress should be considered for the possibility of xanthogranulomatous inflammation. It may also require an aggressive surgical approach [
5-
8].
FUNDING
No funding to declare.
NOTES
-
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
-
AUTHOR CONTRIBUTIONS
S.K.M. participated in data collection and wrote the manuscript. Y.K., J.B.P. and S.H.L. participated in the study design and coordination and helped to draft the manuscript.
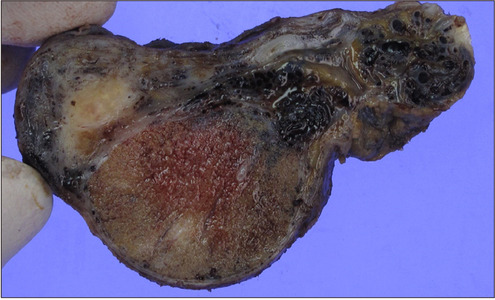
Fig. 1(A) Scrotal ultrasonography: thick-walled heterogeneous lesion in epididymis tail with adjacent edema. (B) Cross-sectional ultrasonography of the epididymis tail: mixed echogenic lesion and hypervascularity. Lt: left.
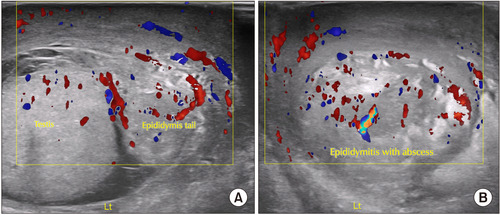
Fig. 2Gross section: the cut surface of the epididymis reveals a yellow nodular lesion measuring up to 1.4 cm in the greatest dimension.
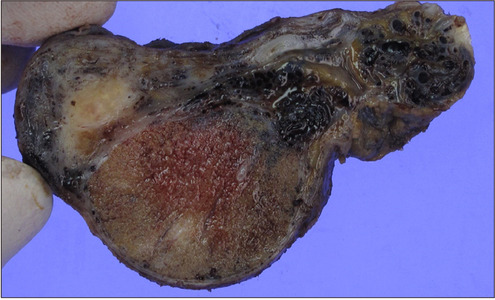
Fig. 3(A) Microscopic section: the epididymis is markedly distorted and replaced with an infiltration of infla-mmatory cells with fibrosis (H&E, ×40). (B) Microscopic section: numerous foamy histiocytes with neutrophils are identified, accompanied by necrotic tissue debris (H&E, ×100).
REFERENCES
- 1. Schaeffer AJ. 2002;Infections of the urinary tract.Article
- 2. Matsuoka K, Yano H, Inoue M, Iida S, Hirabayasi Y, Noda S. Xanthogranulomatous epididymitis. BJU Int 2001;87:275-6. ArticlePubMedPDF
- 3. Kang TW, Lee KH, Piao CZ, Yun KJ, Joo HJ, Park KS, et al. Three cases of xanthogranulomatous epididymitis caused by E. J Infect 2007;54:e69-73. PubMed
- 4. Wiener LB, Riehl PA, Baum N. Xanthogranulomatous epididy-mitis: a case report. J Urol 1987;138:621-2. ArticlePubMed
- 5. Panchal BB, Thakore DH, Tiwari P, Godara N, Kataria D. A rare cause of scrotal abscess: xanthogranulomatous epididymitis. Int Surg J 2023;10:171-4. ArticlePDF
- 6. Won YY, Cha MH, Koh DH, Kim SJ, Joo HJ, Ahn HS. Xanthogranulomatous epididymitis. Korean J Urol 2004;45:613-5.
- 7. Yu DW, Seo IY, Rim JS. Xanthogranulomatous epididymitis associated with bacteremia. Korean J Urol Oncol 2004;2:72-4.
- 8. Kim YJ, Kang SC, Chung JS, Jung YG, Han JY, Suh JK. Xanthogranulomatous epididymitis. Korean J Urol 2006;47:1022-4. Article
- 9. Vijayvergiya G, Gulwani HV, Ul Hasan S. Xanthogranulomatous epididymo-orchitis: a single-institutional case series and systematic review. Indian J Urol 2023;39:58-66. PubMed
- 10. Yamashita S, Umemoto H, Kohjimoto Y, Hara I. Xanthogranulo-matous orchitis after blunt testicular trauma mimicking a testicular tumor: a case report and comparison with published cases. Urol J 2017;14:3094-6.
- 11. Zugor V, Schott GE, Labanaris AP. Xanthogranulomatous pyelonephritis in childhood: a critical analysis of 10 cases and of the literature. Urology 2007;70:157-60. ArticlePubMed
Citations
Citations to this article as recorded by

 , Jun Baek Park
, Jun Baek Park , Sang Hwa Lee1
, Sang Hwa Lee1 , Seung Ki Min2,
, Seung Ki Min2,



 , Department of Urology, Goldman Urology Clinic, 137 Olympic-ro 35-gil, Songpa-gu, Seoul 05510, Korea, Tel: +82-2-421-7511, Fax: +82-2-421-7512, E-mail: msk0701@hanmail.net
, Department of Urology, Goldman Urology Clinic, 137 Olympic-ro 35-gil, Songpa-gu, Seoul 05510, Korea, Tel: +82-2-421-7511, Fax: +82-2-421-7512, E-mail: msk0701@hanmail.net 


 KAUTII
KAUTII
 ePub Link
ePub Link Cite
Cite

