Search
- Page Path
- HOME > Search
Review Articles
- Adult Syphilis: A Narrative Review of Clinical Insights and Public Health Implications in Urology
- Seung-Ju Lee, Jin Bong Choi
- Urogenit Tract Infect 2025;20(3):123-131. Published online December 31, 2025
- DOI: https://doi.org/10.14777/uti.2550039017
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
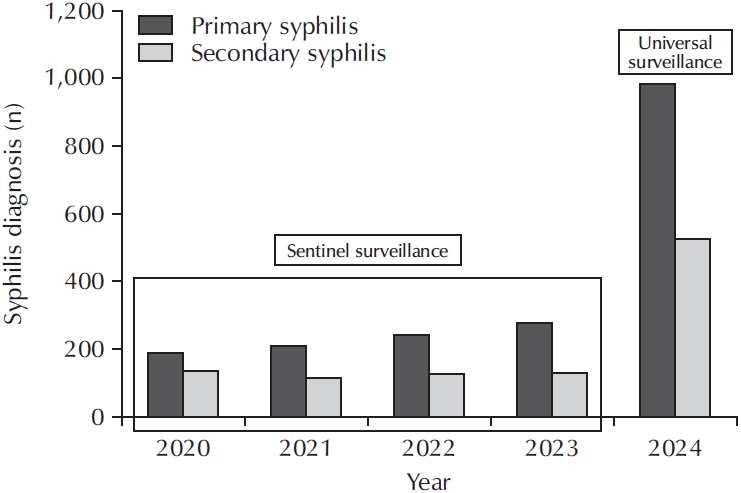
ePub - Syphilis continues to pose a major global public health concern, with more than 7 million cases reported worldwide in 2022, and its incidence continues to rise in numerous regions. In Korea, the shift from sentinel to universal notification in 2024 has revealed a markedly greater disease burden, particularly among men who have sex with men and among younger adults, underscoring changing epidemiological patterns and the urgent need for revised control strategies. In urological practice, syphilis presents with a wide range of often misleading symptoms, including painless genital ulcers, urethritis, and sexual dysfunction, that frequently resemble other genitourinary disorders and complicate diagnostic evaluation. Accurate identification relies on integrating a thorough clinical assessment with serologic testing while remaining alert to diagnostic challenges such as early latent infection, serofast states, and human immunodeficiency virus coinfection. Penicillin G remains the mainstay of therapy, with treatment regimens tailored to the stage of disease and to the presence or absence of central nervous system involvement. Effective partner notification, targeted screening, and consistent follow-up are essential to prevent reinfection and limit further transmission. At a public health level, a multifaceted strategy—strengthened surveillance systems, focused testing in high-risk populations, and embedding syphilis screening within broader sexually transmitted infection care frameworks—is critical to curbing its resurgence. In summary, prompt recognition, adherence to evidence-based management, and coordinated public health measures, together with ongoing advances in diagnostics and prevention, remain fundamental to reducing the continued spread of syphilis and mitigating its impact on both individual and population health.
- 321 View
- 6 Download

- Artificial Intelligence for Autonomous Robotic Surgery in Urology: A Narrative Review
- Dae Young Lee, Hee Jo Yang
- Urogenit Tract Infect 2024;19(3):80-88. Published online December 31, 2024
- DOI: https://doi.org/10.14777/uti.2448020010
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
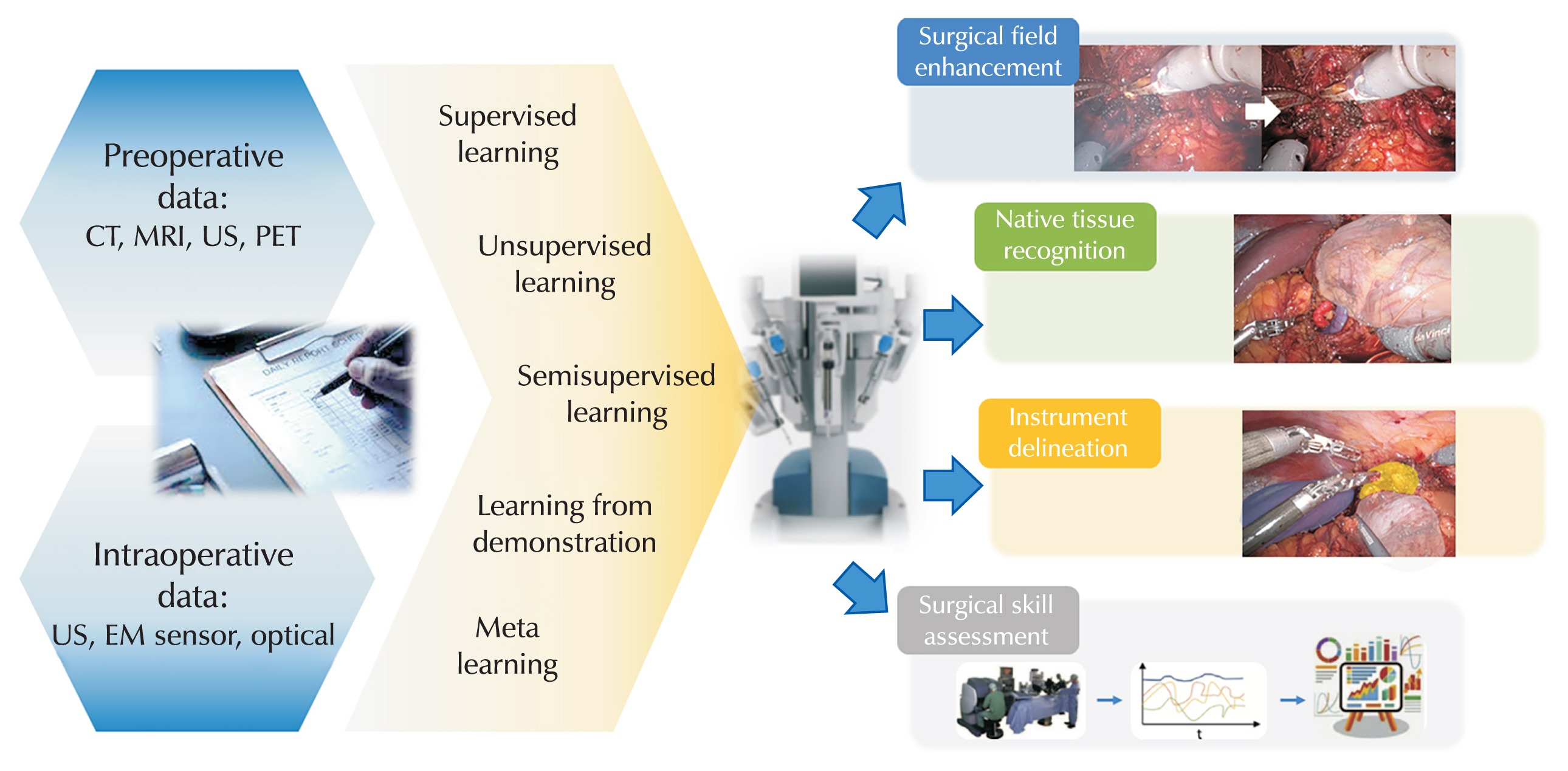
ePub - Artificial intelligence (AI) has emerged as a transformative force in various sectors, including medicine, where it processes high-dimensional data to improve diagnostics and treatment outcomes. This review explores AI applications in urological surgery, highlighting advancements such as image classification and robotic assistance in surgical procedures. AI has demonstrated exceptional diagnostic accuracy, with some systems achieving up to 99.38% in detecting prostate cancer. Additionally, AI facilitates real-time anatomical recognition and instrument delineation, increasing surgical precision. While current robotic systems operate under human supervision, ongoing research aims to advance autonomous surgical capabilities. The future of AI in robotic surgery is promising, especially regarding the possibility of improved outcomes; nonetheless, challenges related to autonomy, safety, and ethics remain.
- 13,094 View
- 162 Download

Reviews
- The Urinary Microbiome: A Pediatric Urological Perspective
- Sang Don Lee, Jae Min Chung
- Urogenit Tract Infect 2022;17(3):61-70. Published online December 31, 2022
- DOI: https://doi.org/10.14777/uti.2022.17.3.61
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - The human microbiome is currently being studied with increasing interest. The microbiome refers to the microorganisms living in the body and their genetic information. The human body is known to contain 1.3 to 10 times more microorganisms than human cells. The Human Microbiome Project was started in 2007 to characterize the human microbiome and analyze its role in human health and diseases. Based on the recent microbiome literature, alterations in the microbiome are associated with several non-urological diseases in pediatrics, such as infantile colic, necrotizing enterocolitis, asthma, atopy, obesity, type-1 diabetes, autism, atopic dermatitis, psoriasis, and bronchial asthma. While some urinary microbiome studies (including prostate cancer, bladder cancer, interstitial cystitis, urge urinary incontinence, overactive bladder, stone disease, and urinary tract infections) have been conducted in adults, there are very few pediatric urinary microbiome studies. This study reviews the role of the urinary microbiome in urinary tract diseases from a pediatric urological perspective.
- 2,574 View
- 16 Download

- The Effects of Short-Chain Fatty Acids in Urological Diseases
- Hee Jo Yang, Doo Sang Kim
- Urogenit Tract Infect 2022;17(1):8-13. Published online April 30, 2022
- DOI: https://doi.org/10.14777/uti.2022.17.1.8
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - The gut microbiome, believed to serve as a second genome within the human body, is involved in the regulation of several metabolic processes. These include human gene expression, development, nutrition and homeostasis. Dysbiosis, is an imbalance in the gut microbiome, which is known to be associated with various disease conditions such as Crohn's disease and Clostridium infections. The gut microbiota communicates with the host through a variety of biomolecules, nutrient signal-independent pathways, and epigenetic mechanisms. The gut microbiota supports the digestion and absorption of food, metabolizes fiber into bioactive short-chain fatty acids (SCFA), produces vitamins and nutrients, maintains gut integrity, and modulates host immunity. Among the above, there has been great interest in SCFA in microbiome research due to its beneficial effects on the intestinal barrier function and systemic anti-inflammatory effects. Recent reports have also indicated the role of SCFA in obesity, insulin resistance, and type 2 diabetes. While SCFA are associated with reduced risk of various diseases, dysbiosis and altered SCFA fermentative pathways could result in disease. This article is a review on the role of SCFA in urological diseases.
-
Citations
Citations to this article as recorded by- Role of microbiome and its metabolite, short chain fatty acid in prostate cancer
Hee Jo Yang, Jae Heon Kim
Investigative and Clinical Urology.2023; 64(1): 3. CrossRef - The Urinary Microbiome; Axis Crosstalk and Short-Chain Fatty Acid
Hee Jo Yang, Doo Sang Kim, Kwang Woo Lee, Young Ho Kim
Diagnostics.2022; 12(12): 3119. CrossRef
- Role of microbiome and its metabolite, short chain fatty acid in prostate cancer
- 2,523 View
- 13 Download
- 2 Crossref


 KAUTII
KAUTII

 First
First Prev
Prev


