Search
- Page Path
- HOME > Search
Review Articles
- Beta-Lactamase-Mediated Antibiotic Resistance in Urinary Tract Infections: Mechanisms and Therapeutic Strategies
- Fanglin Shao, Dengxiong Li, Jie Wang, Zhouting Tuo, Zhipeng Wang, Wuran Wei, Ruicheng Wu, Dechao Feng
- Urogenit Tract Infect 2025;20(2):67-81. Published online August 31, 2025
- DOI: https://doi.org/10.14777/uti.2550012006
-
 Abstract
Abstract
 PDF
PDF PubReader
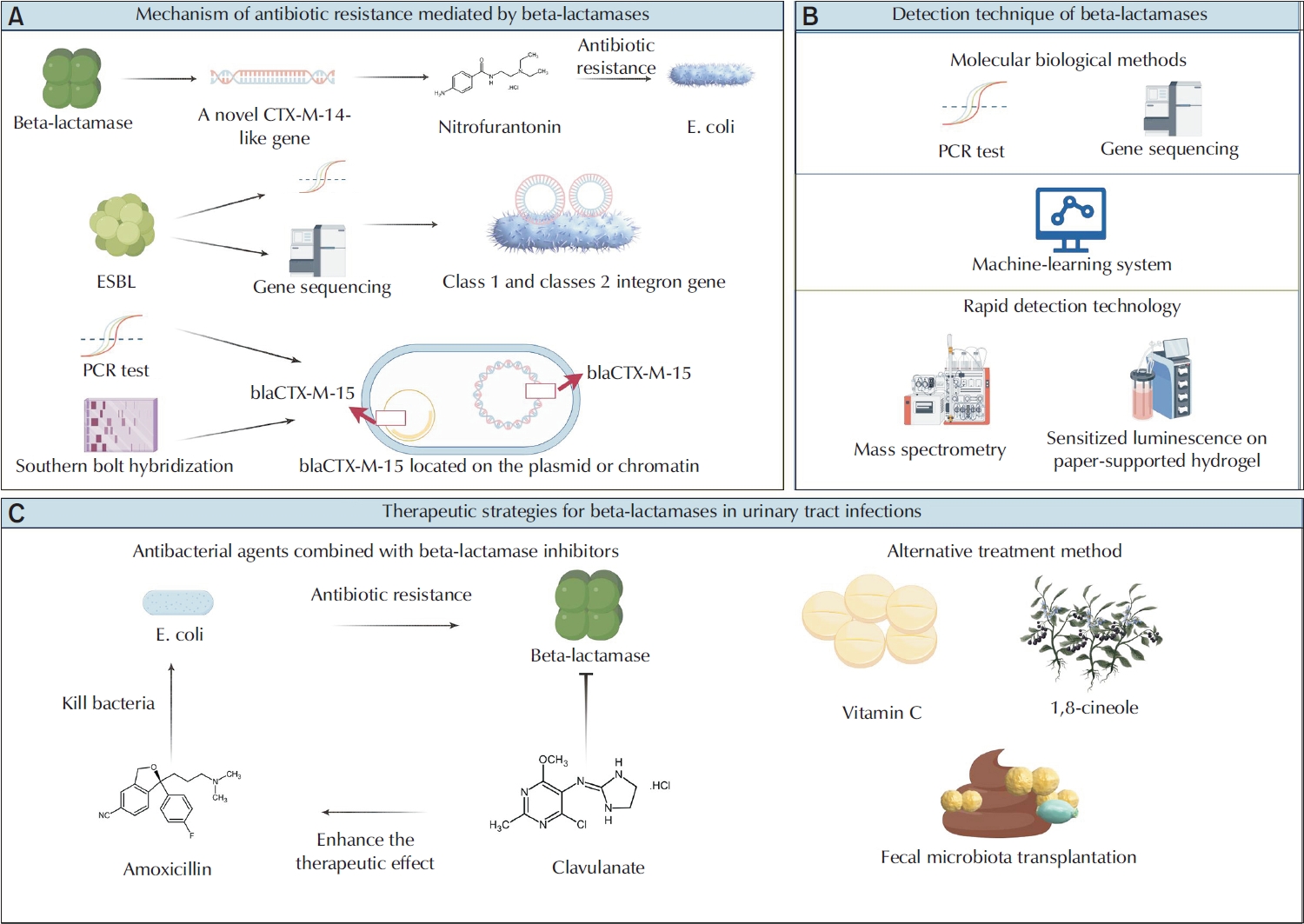
PubReader - Urinary tract infections (UTIs) are among the most prevalent bacterial infections globally, and are primarily caused by Escherichia and Klebsiella. The overprescription and inappropriate use of antibiotics have accelerated the emergence of multidrug-resistant bacteria. Beta-lactamases play a critical role in mediating antibiotic resistance in UTIs. These enzymes promote bacterial resistance through multiple mechanisms, including gene mutation, plasmid-mediated horizontal gene transfer, and the involvement of integrons. Comprehensive knowledge of the ways in which beta-lactamases contribute to resistance in UTIs is essential for improving treatment strategies. Advances in detection technologies, such as gene sequencing and mass spectrometry, have greatly enhanced the ability to monitor and predict bacterial resistance. Current therapeutic strategies include the application of beta-lactamase inhibitors, the development of novel antibiotics, and alternative treatments that have shown efficacy against beta-lactamase-mediated antibiotic resistance. This paper reviews the mechanisms of beta-lactamase-mediated resistance in UTIs and provides an in-depth overview of several detection methods and therapeutic approaches.
-
Citations
Citations to this article as recorded by- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(2): 55. CrossRef
- Editorial for Urogenital Tract Infection (UTI) 2025 Vol. 20 No. 2 – Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 5,604 View
- 68 Download
- 1 Crossref

- Emerging Insights Into Microbiome Therapeutics for Urinary Tract Infections: A Narrative Review
- Hoonhee Seo, Md Abdur Rahim, Indrajeet Barman, Mohammed Solayman Hossain, Hanieh Tajdozian, Fatemeh Ghorbanian, Md Sarower Hossen Shuvo, Jiho Choi, Sukyung Kim, Heejo Yang, Ho-Yeon Song
- Urogenit Tract Infect 2025;20(1):4-16. Published online April 30, 2025
- DOI: https://doi.org/10.14777/uti.2448034017
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Urinary tract infections (UTIs) are among the most common bacterial infections worldwide, affecting millions annually and posing a significant global health concern. Traditional therapies for UTIs are becoming increasingly ineffective due to rising drug resistance and their tendency to disrupt the host's healthy microbiota, leading to further side effects. Consequently, there is an urgent need to develop alternative therapeutic agents that differ from conventional regimens and have fewer or no side effects. In this context, microbiome therapeutics offer a promising solution, given their demonstrated efficacy against various infectious diseases. Advances in scientific technology, particularly next-generation sequencing, have deepened our understanding of urinary microbiome dynamics, revealing a complex interplay within the urobiome that influences the onset and progression of UTIs. Uropathogenic bacteria do not solely cause UTIs; shifts in the composition of the urinary microbiome and interactions within the microbial community, known as host-microbiota interactions, also play a significant role. Although recent studies underscore the potential of targeting the urinary microbiome to manage UTIs and related complications, this field is still emerging and faces numerous regulatory and technical challenges. Further in-depth and comprehensive research is required to advance this pioneering concept into clinical practice.
-
Citations
Citations to this article as recorded by- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
Koo Han Yoo
Urogenital Tract Infection.2025; 20(1): 1. CrossRef - Efficacy and safety of N-acetylcysteine vs. probiotics in in-vivo biofilm prevention on ureteral stents: a prospective randomized controlled pilot in vivo study
Iqbal Singh, Himanshu Agrawal, Shailender Maurya, Himanshu Tanwar, Sanjay Gupta, N. P. Singh
International Urology and Nephrology.2025;[Epub] CrossRef
- Editorial for UTI 2025 Vol. 20 No. 1 - Highlights of This Issue’s Papers and the UTI Editors’ Pick
- 13,543 View
- 155 Download
- 2 Crossref

Original Article
- Characteristics and Treatment Trends for Emphysematous Pyelonephritis in Korea: A 10-Year Multicenter Retrospective Study
- Seung-Kwon Choi, Koo Han Yoo, Jeong Woo Lee, Seung Il Jung, Eu Chang Hwang, Joongwon Choi, Woong Bin Kim, Jung Sik Huh, Jin Bong Choi, Yeonjoo Kim, Jae Min Chung, Ju-Hyun Shin, Jae Hung Jung, Hong Chung, Sangrak Bae, Tae-Hyoung Kim
- Urogenit Tract Infect 2021;16(2):49-54. Published online August 31, 2021
- DOI: https://doi.org/10.14777/uti.2021.16.2.49
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Purpose: This study examined the characteristics, current treatment trends, and outcomes of patients with emphysematous pyelonephritis (EPN) in Korea.
Materials andMethods: Two hundred and seventeen patients diagnosed with EPN were evaluated using abdominal computed tomography in 2011-2021 at 15 institutes in Korea. The patients’ demographic and clinical characteristics, treatment modalities, and treatment outcomes were analyzed. The total study period was divided arbitrarily into groups A (2011-2014), B (2015-2017), and C (2018-2021) to analyze the trends in the EPN treatment.
Results: The mean age of the patients was 65.1 years; there were more female patients (74.2%) than male patients. The overall mortality rate was 10.6%. Ninety-five (43.8%), 98 (45.2%), and 24 (11.0%) patients were treated with medical, minimally invasive, and surgical management, respectively; the corresponding mortality rates were 13.7%, 6.1%, and 16.7%. There was no significant change in the proportion of patients treated with medical management over time (group A=46.5%, group B=47.0%, and group C=38.8%). The proportion of patients treated with minimally invasive management gradually increased over time (group A=35.2%; group B=43.9%; group C=55.0%), while those who underwent surgical management decreased gradually over time (group A=18.3%, group B=9.1%, and group C=6.3%). No differences in mortality rates were observed between the groups.
Conclusions: EPN with medical and minimally invasive management had a relatively high treatment success rate, which increased gradually, while surgical management decreased gradually over time in Korea. The mortality rate was relatively lower than that reported in studies published before the 2010s.
- 1,765 View
- 7 Download

Review
- UPOINT System: A Diagnostic/Therapeutic Algorithm for Chronic Prostatitis/Chronic Pelvic Pain Syndrome
- Phil Hyun Song
- Urogenit Tract Infect 2020;15(2):27-32. Published online August 31, 2020
- DOI: https://doi.org/10.14777/uti.2020.15.2.27
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader ePub
ePub - Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) is a common condition that significantly affects the quality of life. On the other hand, urologists find it challenging to treat this disorder effectively. To date, the Urinary, Psychosocial, Organ-Specific, Infection, Neurological/Systemic, and Tenderness (UPOINT) system is the only classification tool that can improve the treatment outcomes significantly compared to monotherapy. This review focused on the most recent advances in the diagnosis and treatment of CP/CPPS.
-
Citations
Citations to this article as recorded by- Treatment Modality of Prostatic Abscess according to Size: A Retrospective Study
Gwon Kyeong Lee, Kyoung Ha Jang, Woo Seop Seong, Byeong Jin Kang, Kyung Hwan Kim, Hong Koo Ha
Urogenital Tract Infection.2022; 17(3): 96. CrossRef
- Treatment Modality of Prostatic Abscess according to Size: A Retrospective Study
- 8,831 View
- 61 Download
- 1 Crossref


 KAUTII
KAUTII

 First
First Prev
Prev


